Survey on sufferers’ perspective in direction of the dietary counselling within the dental setting
Three-hundred thirteen patients (123 males and 190 females) participated in the survey (mean age: 53 ± 17 years; range: 18–87 years). In Group 1 (dental setting: private practice), questionnaires were filled by 109 patients (mean age: 51 ± 15 years; range: 18–82 years; 24 males and 85 females). In Group 2 (dental setting: healthcare system within the hospital), questionnaires were filled by 104 patients (mean age: 53 ± 18 years; range: 21–80 years; 50 males and 54 females). Group 3 (dental setting: intra moenia private practice within the hospital) included 100 questionnaires (mean age: 54 ± 19 years; range: 19–87 years; 51 females and 49 males).
Table 1 summarizes the main patients’ socio-demographic data at baseline, divided into three different settings.
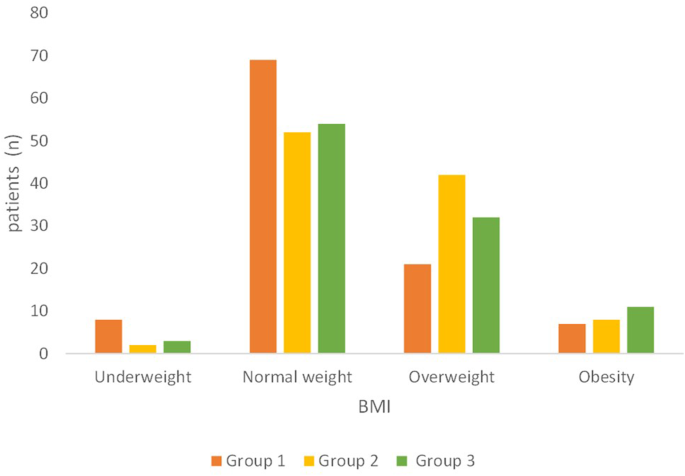
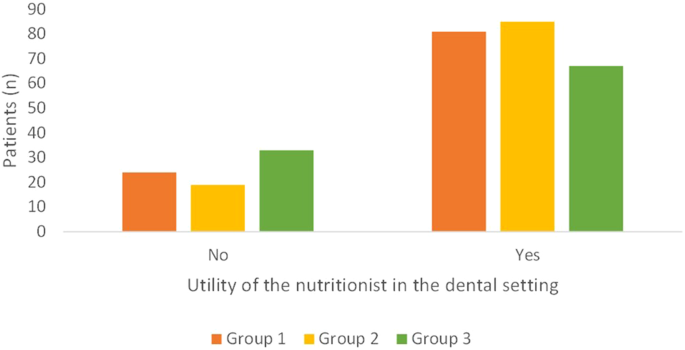
Most of the patients showed a BMI within the range of normality (p = 0.02; Fig. 1). Group 1 had the higher number of underweight patients (n = 8), while Groups 2 and 3 showed the highest number of overweight or obese patients (n = 50 and n = 43, respectively).
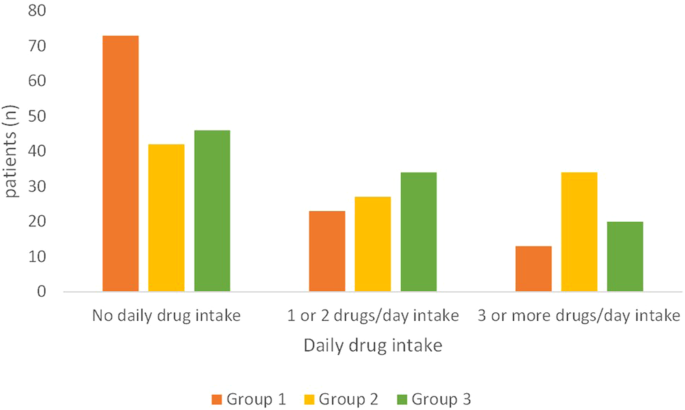
Most of the patients in Group 1 (private practice) reported to not take medications daily (mean= 0.7 ± 1.2 medications/day; range: 0–7 medications) (Fig. 2). In Group 2 (hospital healthcare system) and Group 3 (private practice within the hospital, intra-moenia), most patients had an intake of one or more medications daily (mean= 1.8 ± 2.1 medications/day with a range of 0–10 medications and mean = 1.5 ± 2.4 medications/day with a range of 0–10 medications, respectively) (Fig. 2). Group 2 showed a higher number of patients taking 3 or more drugs/day (p < 0.01; Fig. 2).
Answers to the questionnaire
“Have you ever followed a diet?”
This question provides an indication of the previous patient’s propensity and sensibility to receive nutritional counselling. In all the groups, around half of the patients reported to have followed a diet: 63 patients in Group 1, 57 patients in Group 2, and 47 patients in Group 3, without significant differences (p = 0.28). In most of cases, the diet was prescribed by a dietician, a nutritionist, or a clinician, while only in a few cases the diet was self-made (Group 1, n = 10; Group 2, n = 22; Group 3, n = 23). In Group 1, the patients who already followed a diet were predominantly females (8 males and 38 females), while, in the other groups, the sexes were balanced.
In Group 1, 15 patients out of 63 (23.8%) who had already received a diet had a BMI out of range: 3 of them were obese (class I n = 1; class II n = 1; class III n = 1) and 11 were overweight, while 1 patient was slightly underweight. Among the patients who reported never having received a diet (n = 46), a significantly higher number of patients (n = 21; 45.6%; p = 0.02) recorded a BMI out of range compared to the patients who already had a diet: 10 patients were overweight, 4 were obese (class I n = 2; class II n = 2) and 7 were slightly underweight.
In Group 2, 30 patients out of 47 (63.8%) that had already received a diet showed a BMI out of range (three were in class I obesity; 27 patients were overweight). They were significantly more than patients who had not received a diet with a BMI out of range (n = 22 out of 57, 38.5%; p = 0.02; 15 were overweight, five were in class I obesity, and two were slightly underweight).
In Group 3, 29 patients out of 53 (54.7%) that already received a diet had a BMI out of range (twenty were overweight, six were in class I obesity, two in class II obesity, one was slightly underweight), and, among the 47 patients without having received a previous diet, 17 of them (36.1%; p = 0.17) had a BMI out of range (twelve were overweight, two were in class I obesity, one was in class II obesity, one was slightly underweight, one was visibly underweight).
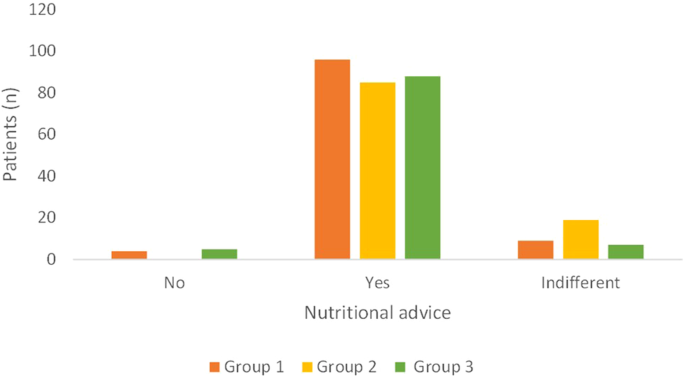
“Would you like to receive advice on nutrition, both in general and, specifically, to prevent oral diseases, such as periodontitis, tooth decay and oral cancer?”
Most patients (>80%) reported their willingness to receive information regarding nutrition in all the three Groups (Fig. 3; p = 0.01). Among the patients who were not interested in having nutritional advice, two were underweight in Group 1, while, in Group 3, one was overweight and one was in class I obesity. Group 2 showed a higher number of patients “indifferent” to receiving the nutritional advice.
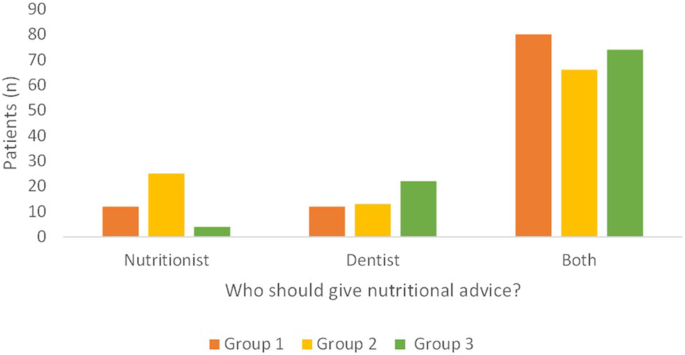
“Do you think a dentist, a nutritionist or both should provide such advice to you?”
In Group 1, 5 patients did not reply to this question; thus, only 94 answers were collected.
The majority of patients, in all the Groups, identified both the dentist and the nutritionist having the role of providing advice (Fig. 4; p < 0.01). In few cases, the role of the dentist alone or the nutritionist alone was recognized, with no difference between the two figures for the Group 1, while the Group 2 recognized the role of the nutritionist more than the Group 3, which reported a predominant importance of the dentist (Fig. 4; p = 0.0002).
“Do you think the figure of the nutritionist can be useful in the dental clinics?”
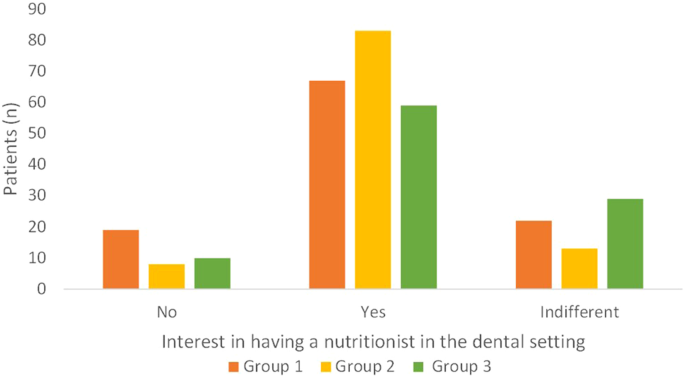
In all groups, the nutritionist was perceived as useful by most patients in the dental setting, particularly in Group 2, which had patients from the healthcare system (Fig. 5; p = 0.05).
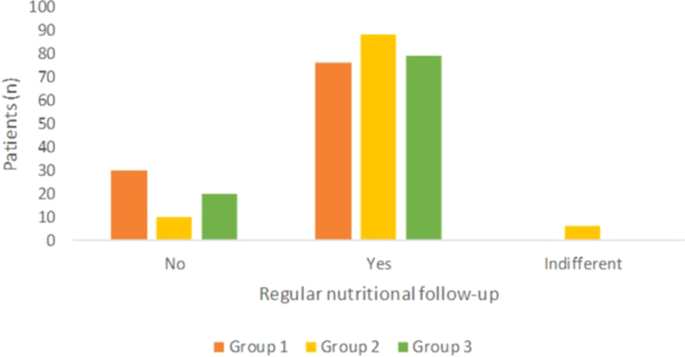
“Could you be interested in having, at the dental clinic you are referring to, a nutritionist who can give advice on nutrition in general, also providing a diet useful for managing and preventing diseases other than those of the mouth (systemic diseases, such as diabetes or cardiovascular disorders)?”
Most patients expressed interest in having an expert nutritionist at the dental clinic they refer to (Fig. 6; p < 0.01). This was significantly more evident in Group 2, where more than 80% of patients answered positively to this item (Fig. 6; p = 0.003). Among the patients who were not interested in having a nutritionist within the dental setting, 8 patients had a BMI out of range in Group 1 (four were overweight; two were in class I obesity; one was in class II obesity; one was slightly underweight); 4 patients were overweight in Group 2; 8 patients in Group 3 were out or range (six were overweight; two were in class I obesity).
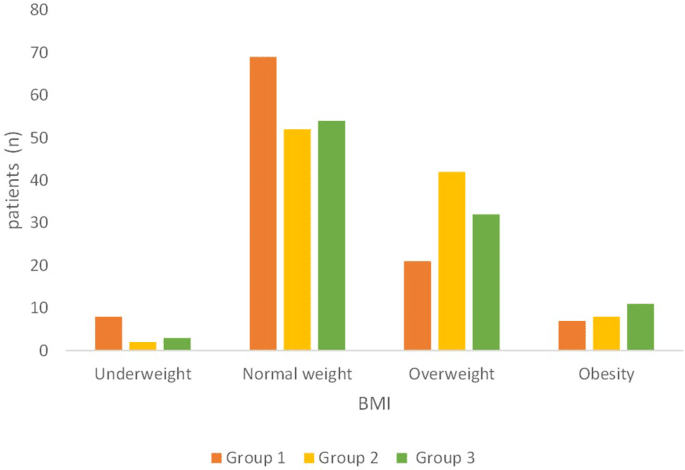
“In addition to planning a diet, do you think it would be useful to set a regular follow-up with the nutritionist to monitor the achievements of the dietary goals?”
Planning regular nutritional follow-up was recognized as valuable by most patients, especially in Group 2, where patients responded positively in more than 80% of cases. (Fig. 7; p < 0.01).